I’m putting this into our Women: Going Well section with a clear understanding that a lot more work is needed. However the fact that there’s some work happening to research women’s health is a positive. We’ll take it where we can it, right?
In 1993, the U.S. mandated that women and minorities be included in clinical trials funded by the federal government. More than 20 years later, it has become clear just how critical that law was: Studies have shown that not only do men and women experience certain diseases differently, but also their response to treatments can vary considerably.
Paula Johnson, professor of medicine at Harvard Medical School and executive director of the Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital in Boston, says what researchers have learned so far is only the tip of the iceberg.
“The entire field of sex and gender-based medicine is so underrecognized as an important lens through which to consider science, care and how we think about exposure to health risks,” Dr. Johnson says. “There’s a huge amount of work to do.”
Here are some of the important discoveries that have come out of gender-based research over the past two decades:
Alzheimer’s. Two-thirds of the 5.1 million Alzheimer’s patients in the U.S. are women. For years, researchers assumed that more women develop Alzheimer’s simply because the disease is associated with age, and women live longer than men. Recent research, however, has indicated that hormones may play a role. Animal studies have connected a lack of estradiol—a form of estrogen that affects the brain—with risk factors for Alzheimer’s, leading researchers to delve into the role ovarian decline may play in the deterioration of the brain as women age. The research is in its infancy, but scientists hope it ultimately will shed light on whether and how gender plays a role in both the development of Alzheimer’s and the severity of the symptoms. Meanwhile, gender-based studies already have led to clinical trials of two drugs that are being tested equally on men and women.
Nicotine addiction. Women tend to become addicted to nicotine more easily than men, and research has indicated that the strategies typically employed to help people stop smoking, such as patches, pills or nasal sprays, are less effective for women than men. Studies show that women tend to have more success with a chewing strategy, so doctors trying to help women quit smoking might be better off recommending nicotine gums than any of the other options. But because it takes a while for research to be translated into clinical treatment, this sort of gender-based approach isn’t yet common.
Lung cancer. Women are also at a high risk for lung cancer. It kills more women each year than breast, ovarian and uterine cancers combined, but not because of the female predilection for nicotine. In fact, the disease is strikingly prevalent in nonsmoking females. Researchers have found that hormones, particularly estrogen, influence lung-cancer development and mortality. In addition to making women metabolize nicotine more quickly than men, estrogen triggers the estrogen receptors that are present on 45% to 70% of lung cancers, and may also play a role in activating certain genes within tumors that could affect whether cancer responds to treatment.

Inclusion of women in clinical trials of various lung-cancer treatments has shown that women respond differently to treatments than men. The most clear-cut example of this is a new set of targeted cancer therapies—particularly the use of tyrosine-kinase inhibitors—that seem to help women more than men. So far, this research hasn’t made its way out of the lab, but all signs point to the eventual prescription of treatments along gender lines.
Pain. Researchers have long known that men and women experience pain differently. As it turns out, females process pain in a different part of the brain than males, and they are more sensitive to it, which may be why more women suffer from chronic-pain conditions such as arthritis and fibromyalgia. And yet men and women typically are treated equally when it comes to pain management. However, new research indicates that pain also activates different immune cells in the sexes, a discovery that could lead to more effective pain treatments for both.
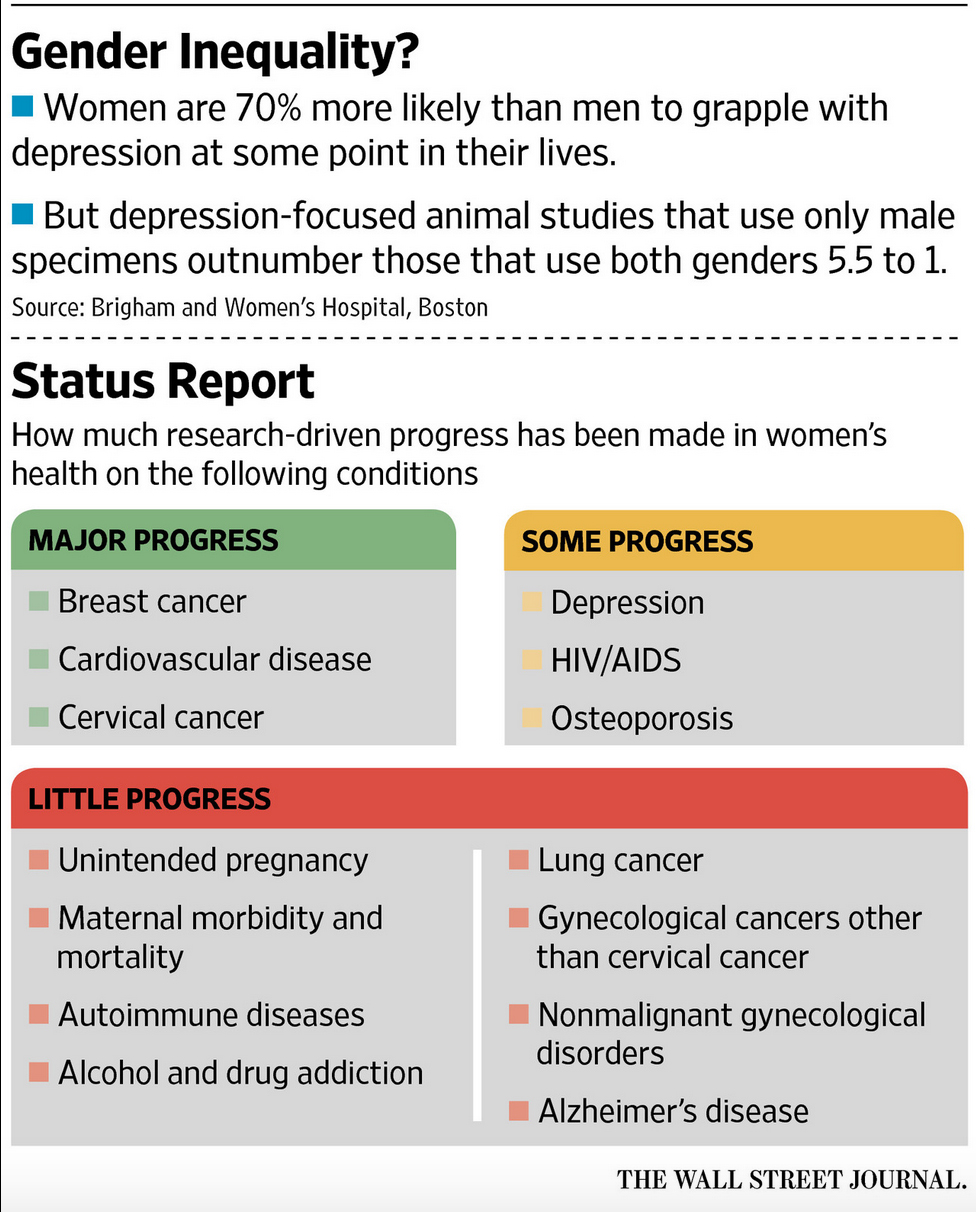
Depression. In the U.S., twice as many women as men currently suffer from depression, and women are 70% more likely to grapple with depression at some point in their lives. Researchers still have very little understanding of why that is, and more research is needed on that front. They do know, however, that the drugs used to treat depression interact very differently with the female body. Women have different enzymes, meaning they metabolize drugs differently than men. Hormonal fluctuations can further affect metabolism, and female hormones such as estradiol and progesterone interact with various neurotransmitters in the brain—including dopamine and serotonin—which can further affect treatment outcomes. Hormonal changes throughout a woman’s life, including puberty, pregnancy and menopause, have been directly linked with depression.
Recent clinical trials of antidepressants have included higher percentages of women and are starting to shed some light on how sex differences might influence treatment. Still, despite the fact that it has been well-established that sex hormones play a role in a variety of mental disorders (women are also twice as likely to suffer from anxiety), animal studies that rely solely on male specimens continue to outnumber those that include both genders 5.5 to 1.